Indications for Cardiac MRI
1. Heart Failure
|
CMR provides an excellent clinical investigation in patients with new diagnosis or worsening of heart failure.
CMR is helps to: 1. clarify the underlying aetiology
3. monitor improvement of cardiac volumes with anti-remodelling therapy (changes in ESV in heart failure) 4. risk stratification by the presence of myocardial scar and native T1 5. guide device therapy by :
|
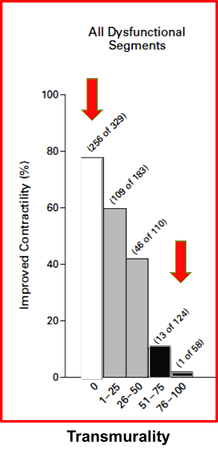
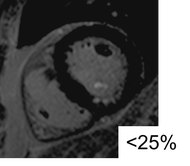
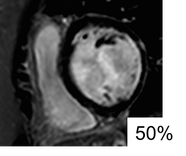
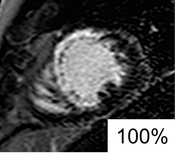
Clinical significance of transmurality of ischaemic scar in predicting improvement in contractile function with coronary revascularization. From Kim et al 2000
|
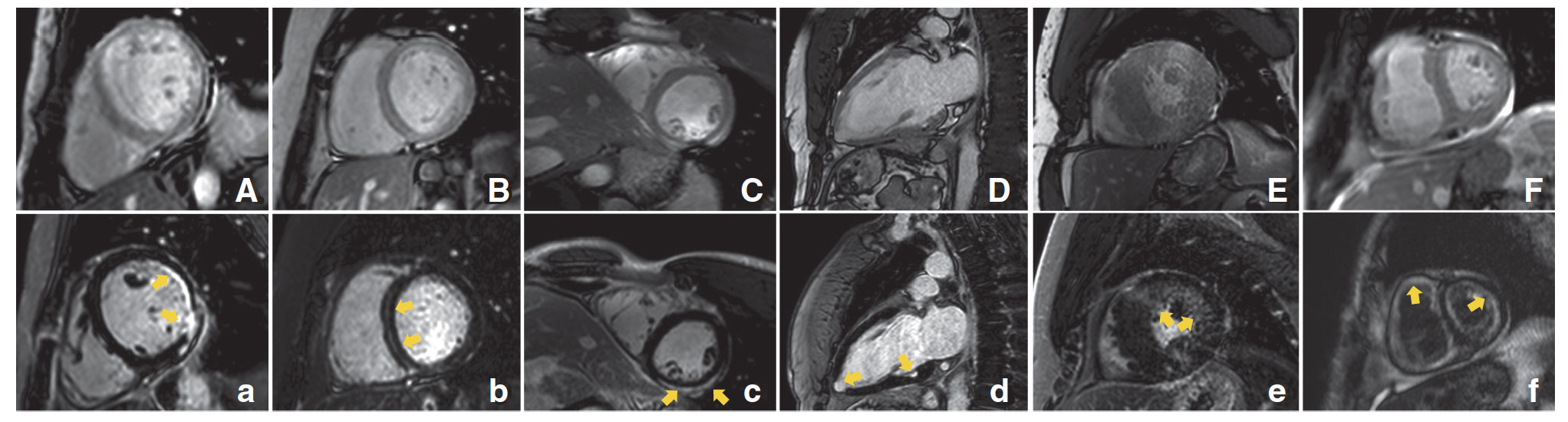
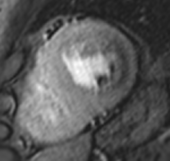
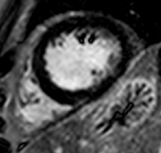
LGE patters in deciphering underlying aetiology in HF. A, Ischemic cardiomyopathy with subendocardial LGE in the antero- and inferolateral wall. B, Idiopathic dilated cardiomyopathy with mid-myocardial striae of LGE. C, Acute myocarditis with subepicardial LGE in the infero-lateral wall. D, Cardiac sarcoid with multiple focal areas of LGE (2CH view, particularly, in the inferior wall and apex). E, Hypertrophic cardiomyopathy with diffuse and circumferential LGE. F, Cardiac amyloid with diffuse and subendocardial enhancement. From: Puntmann et al. 2016
2. Chest pain - Angina Pectoris
|
1. Stable angina (chronic chest pain)
stress-myocardial perfusion is the ultimate diagnostic test for the presence and relevance of myocardial ischaemia
2. Patients presenting with ACS
2. Patients presenting with ACS
|
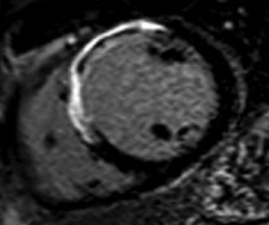
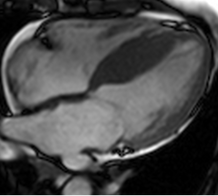
Adenosine stress test reveals a significant myocardial perfusion defect in basal-apical inferolateral segments. In the absence of myocardial scar in the LGE images, this finding speaks for relevant myocardial ischaemia. Left: adenosine perfusion, right: LGE.
Midventricular slice
Apical slice
|
3. Cardiomyopathies
|
Specific cardiomyopathies
1. Left ventricular hypertrophy
8. Suspected infiltrative disease (?amyloidosis) 9. Patients at risk of cardiac iron loading (chronic transfusions) 10. Right ventricular enlargement
Guidelines recommendations: ESC Evidence level II (B), US: A |
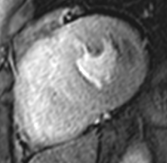
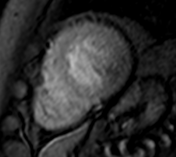
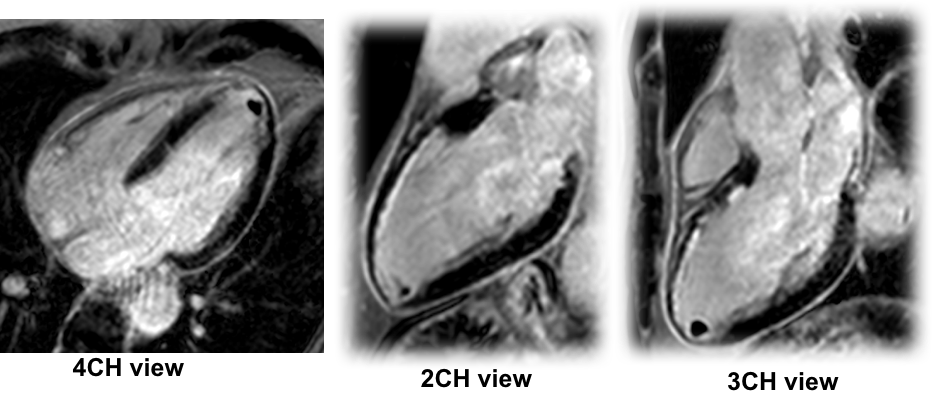
Hypertrophic cardiomyopathy. A. Cine 4CH view: asymmetric septal hypertrophy. B. LGE: evidence of scar in superior RV insertion point, From Puntmann et al. 2013.
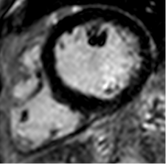
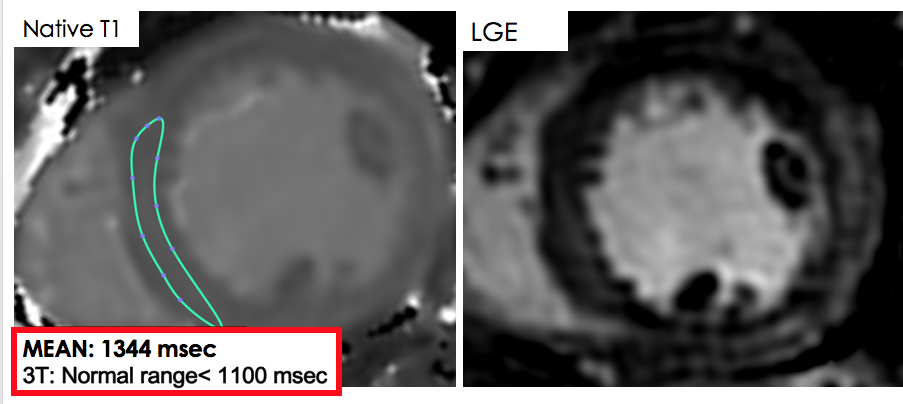
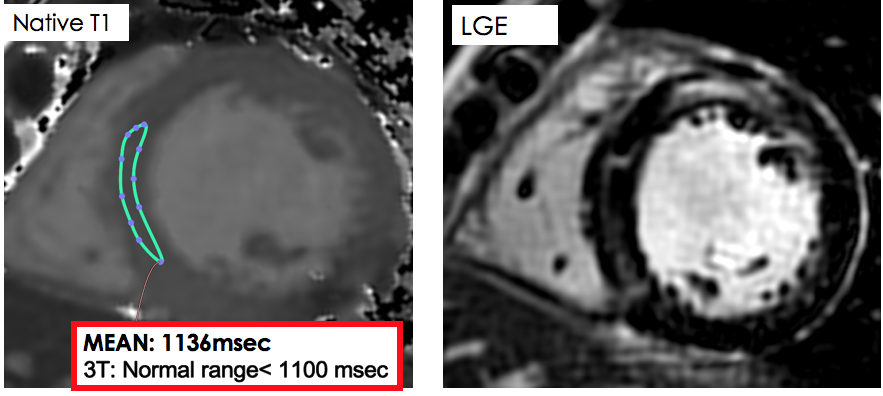
Acute myocarditis. A. Native T1 is highly elevated (>5SD). There is only a hint of diffuse LGE in the inferolateral segments. From Hinojar et al 2015
Chronic myocarditis. A. Native T1 is only mildly abnormal (>2SD). There is residual non-ischaemic intramyocardial scar in the anterior segments.
|
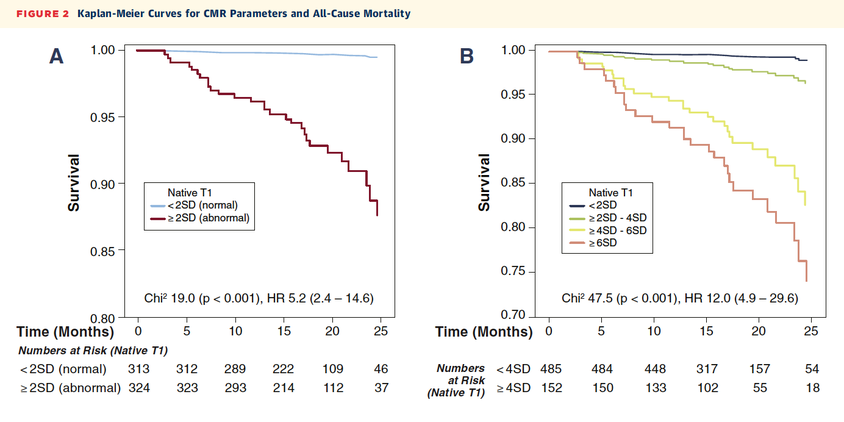
Native T1 and all-cause mortality in non-ischaemic dilated cardiomyopathy. From Puntmann et al. 2016
4. Cardiac Masses and Thrombi
5. Pericardial disease1. Pericardial effusion
2. Pericarditis
A- appropriate (US appropriateness criteria); I - level of recommendation for an indication (ESC guidelines)
|
6. Valvular disease1. Aortic stenosis:
|
Overview on CMR indications in ESC guidelines (Von Knobelsdorff-Brenkenhoff F et al, JCMR 2016).